What are endocrine disruptors?
Endocrine disruptors (EDs) are chemicals that can interfere with the endocrine (hormone) system in mammals at certain doses. They are found in many household and industrial products and are sometimes also referred to as hormonally active agents, endocrine disrupting chemicals, or endocrine disrupting compounds (EDCs).
Such substances may disrupt the synthesis, secretion, transport, binding, action, or elimination of natural hormones in the body that are responsible for development, behavior, fertility, and maintenance of homeostasis (normal cell metabolism). These disruptions can increase the risk of cancerous tumors, birth defects, and other developmental disorders.
Any system in the body controlled by hormones can be disrupted by hormone disruptors. The critical period of development for most organisms is between the transition from a fertilized egg into a fully formed infant. As cells begin to grow and differentiate, there are critical balances of hormones and protein changes that must occur. Although a dose of disrupting chemicals may do substantial damage to a developing fetus, the same dose may not significantly affect the adult mother.
Studies in cells and laboratory animals have shown that EDs can cause adverse biological effects in animals. Low-level exposures may also cause similar effects in human beings. The term endocrine disruptor is often used as synonym for xenohormone, although the latter can mean any naturally occurring or artificially produced compound showing hormone-like properties (usually binding to certain hormonal receptors). EDCs in the environment have been linked to reproductive and infertility problems in wildlife, and bans and restrictions on their use have been associated with a reduction in health problems and recovery of some wildlife populations.
Where are EDs found?
- Household and industrial products
- Drugs
- Herbicides and pesticides
- Compounds used in the plastics industry and in consumer products
- Industrial by-products and pollutants
- Some naturally produced botanical chemicals
Some endocrine disrupting compounds are pervasive and widely dispersed in the environment and may bio-accumulate. Some are persistent organic pollutants (POP’s) which can be transported long distances across national boundaries and found in virtually all regions of the world, including near the North Pole, due to weather patterns and cold conditions. Others are rapidly degraded in the environment or human body or may be present for only short periods of time.
EDs can disrupt organ function in our bodies by:
- Increasing or decreasing production of certain hormones
- Imitating hormones
- Turning one hormone into another
- Interfering with hormone signaling
- Promoting premature cell death
- Competing with essential nutrients
- Binding to essential hormones
- Accumulating in organs that produce hormones
Health effects attributed to endocrine disrupting compounds include:
- Reproductive problems (reduced fertility, male and female reproductive tract abnormalities, skewed male/female sex ratios, loss of fetus, menstrual problems)
- Sexual development problems such as feminizing of males or masculinizing effects on females, etc.
- Changes in hormone levels
- Early puberty
- Impaired immune functions
- Cognitive, behavioral, and other brain development problems
- Learning disabilities
- Severe attention deficit disorder (ADHD)
- Deformations of the body (including limbs)
- Various cancers, including cancer of the breast, prostate, thyroid
The 12 worst endocrine disrupters are known as the “Dirty Dozen List of Endocrine Disruptors”and include:
- Bisphenol-A (BPA)
- Dioxin
- Atrazine
- Phthalates
- Perchlorate
- Fire retardants
- Lead
- Arsenic
- Mercury
- Perfluorinate chemicals
- Organophosphate pesticides
- Glycol ethers
Tips to avoid these hormone disrupters:
- Bisphenol-A (BPA): A chemical used in plastics which imitates the sex hormone estrogen in your body. BPA has been linked to breast and other cancers, reproductive problems, obesity, early puberty, and heart disease. According to government tests, 93 % of Americans have BPA in their bodies! Avoid it: BPA is commonly found in plastic bottles, plastic food containers, dental materials, the linings of metal food and infant formula cans, and thermal paper receipts commonly used at grocery stores and restaurants, because the paper is commonly coated with a BPA-containing clay for printing purposes. Select fresh food instead of canned, since many food cans are lined with BPA. Otherwise, find out which companies avoid BPA or similar chemicals in their products. Avoid receipts when possible, or store them in a plastic bag. Avoid plastics marked with a “PC,” for polycarbonate, or recycling label #7. While not all of these plastics contain BPA, many do.
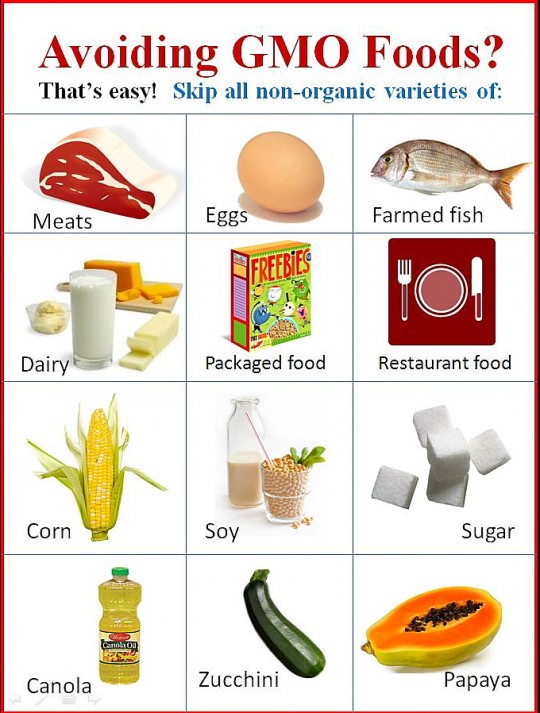
- Dioxins: Chemicals which form during many industrial processes when chlorine or bromine are burned in the presence of carbon and oxygen. Dioxins can disrupt the delicate way that male and female sex hormone signaling occurs in the body. Exposure to low levels of dioxin in the womb and early in life can permanently affect sperm quality and lower sperm count in men during their prime reproductive years. Additionally, dioxins are very long-lived, powerful carcinogens, build up in both the body and food chain, and can affect the immune and reproductive systems. Avoid it: A difficult task, since the ongoing industrial release of dioxin has caused the American food supply to become widely contaminated. Products including meat, fish, milk, eggs, and butter are most likely to be contaminated. Reduce your exposure by eating fewer animal products.
- Atrazine: The introduction of highly toxic chemicals into nature has contributed to the feminization of male frogs. Exposure to even low levels of the herbicide atrazine can turn male frogs into females that produce completely viable eggs. Atrazine is widely used on the majority of corn crops in the United States and has become a pervasive drinking water contaminant. It has been linked to breast tumors, delayed puberty, and prostate inflammation in animals. Some research has linked it to prostate cancer in people. Avoid it: Buy organic produce and get a drinking water filter certified to remove atrazine. (For a good filter, see EWG’s buying guide: www.ewg.org/report/ewgs-water-filter-buying-guide/).
- Phthalates: Found in some soft toys, flooring, medical equipment, cosmetics, and air fresheners, phthalates are known to disrupt the endocrine system of animals. Some research has implicated them in the rise of birth defects of the male reproductive system and possibly the reproductive system of infants. California and Europe have both banned them from toys. One phthalate, Bis(2-ethylhexyl) phthalate (DEHP), used in medical tubing, catheters and blood bags, may harm sexual development in male infants. In 2002, the Food and Drug Administration (FDA) released a public report which cautioned against exposing male babies to DEHP due to it’s possible effects on the development of the male reproductive system and production of normal sperm in young animals. Phthalates may also play a causal role in disrupting masculine neurological development when exposed prenatally. A specific signal programs cells in our bodies to die. It’s totally normal and healthy for 50 billion cells in your body to die every day! But studies have shown that phthalates can trigger “death-inducing signaling” in testicular cells, making them die earlier than they should. Studies have also linked phthalates to hormone changes, lower sperm count, less mobile sperm, birth defects in the male reproductive system, obesity, diabetes and thyroid irregularities! Avoid it: Avoid plastic food containers, children’s toys (some phthalates are already banned in kid’s products), and plastic wrap made from PVC, which has the recycling label #3. Some personal care products also contain phthalates, so read labels and avoid products that simply list added “fragrance,” since this catch-all term often means hidden phthalates. (For phthalate-free personal care products, see EWG’s Skin Deep Database: www.ewg.org/skindeep/).
- Perchlorate: A component in rocket fuel, this contaminates much of our produce and milk, according to EWG and government test data. When perchlorate gets into your body, it competes with the nutrient iodine which the thyroid gland needs to make thyroid hormones. Ingesting too much of it can alter your thyroid hormone balance. This is important, since it is these hormones that regulate metabolism in adults and are critical for proper brain and organ development in infants and young children. Avoid it: Reduce perchlorate in drinking water by installing a reverse osmosis filter (www.ewg.org/report/ewgs-water-filter-buying-guide). It is difficult to avoid perchlorate in food, but you can reduce its potential effects on you by including enough iodine in your diet by eating seafood, produce grown in soil containing iodine, and iodized salt.
- Fire retardants: In 1999, Swedish scientists discovered that women’s breast milk contained an endocrine-disrupting chemical found in fire retardants, and the levels had been doubling every five years since 1972! These incredibly persistent chemicals, known as polybrominated diphenyl ethers or PBDEs, have since been found to contaminate the bodies of people and wildlife around the globe. PBDEs can imitate thyroid hormones in our bodies and disrupt their activity. That can lead to lower IQ, among other significant health effects. While several kinds of PBDEs have been phased out, PBDEs are incredibly persistent and will contaminate people and wildlife for decades to come. Avoid it: It’s virtually impossible, but passing better toxic chemical laws that require chemicals to be tested before they go on the market would help reduce our exposure. Use a vacuum cleaner with a HEPA filter, which can cut down on toxic-laden house dust; avoid reupholstering foam furniture; take care when replacing old carpet (the padding underneath may contain PBDEs). (More tips: www.ewg.org/pbdefree/).
- Lead: A heavy metal, lead is toxic especially to children, harms almost every organ system in the body, and has been linked to numerous health effects, including permanent brain damage, lowered IQ, hearing loss, miscarriage, premature birth, increased blood pressure, kidney damage, and nervous system problems. Lead also disrupts your hormones. In animals, lead has been found to lower sex hormone levels. Research indicates that lead can disrupt the hormone signaling that regulates the body’s major stress system (HPA axis). This stress system is implicated in high blood pressure, diabetes, anxiety and depression. Avoid it: Keep your home clean and well maintained. Crumbling old paint is a major source of lead exposure, so remove it carefully. A good water filter can reduce exposure to lead in drinking water. Studies have shown that children with healthy diets absorb less lead.
- Arsenic: A highly toxic substance used since the 1940’s in food animals and recently discovered in drinking water and various crops. In 2010, about 88% of the approximately 9 billion chickens in the United States raised for meat were administered arsenic-based feed additives. Why? Arsenic has antimicrobial properties which help to kill parasites, promotes weight gain, and improves the color of chicken flesh to make it more appealing to humans. In small amounts, arsenic can cause skin, bladder, and lung cancer and disrupt hormones. In larger amounts it can kill you! Arsenic can also interfere with normal hormone functioning in the glucocorticoid system that regulates how our body processes sugars and carbohydrates. Disrupting the glucocorticoid system has been linked to weight gain/loss, protein wasting, immunosuppression, insulin resistance (which can lead to diabetes), osteoporosis, growth retardation, and high blood pressure. Avoid it: Select organic poultry or poultry raised naturally without antibiotics. Reduce your exposure by using a water filter that lowers arsenic levels. (www.ewg.org/report/ewgs-water-filter-buying-guide/).
- Mercury: A naturally occurring but toxic metal, mercury enters the air and oceans primarily though burning coal. Eventually, it can end up on your plate in the form of mercury-contaminated seafood. Pregnant women are most at risk from mercury’s toxic effects, since the metal is known to concentrate in the fetal brain and interfere with brain development. Mercury is also known to bind directly to one particular hormone that regulates a woman’s menstrual cycle and ovulation, interfering with normal signaling pathways. The metal may also play a role in diabetes, since it has been shown to damage insulin-producing cells in the pancreas which are critical for the body’s ability to metabolize sugar. Avoid it: For people who want to eat sustainable seafood with lots of healthy fats, but without a side of toxic mercury, wild salmon, herring, sardines, and farmed trout are good choices.
- Perfluorinated chemicals (PFCs): Perfluorochemicals used to make non-stick cookware are so widespread and persistent that 99 % of Americans have these chemicals in their bodies. One particularly notorious compound called PFOA has been shown to be “completely resistant to biodegradation” and will never break down in the environment! Although the chemical was banned after decades of use, it will persist in people’s bodies for countless generations to come. PFOA exposure has been linked to decreased sperm quality, low birth weight, kidney disease, thyroid disease, high cholesterol, and other health problems. Animal studies have found it to disrupt thyroid and sex hormone levels. Avoid it: Avoid non-stick pans, as well as, stain- and water-resistant coatings on clothing, furniture, and carpets.
- Organophosphate pesticides: Neurotoxic organophosphate compounds that the Nazis produced in huge quantities for chemical warfare during World War II were luckily never used. After the war ended, American scientists used the same chemistry to develop a long line of pesticides that target the nervous systems of insects. Despite many studies linking organophosphate exposure to effects on brain development, behavior, and fertility, they are still among the more common pesticides in use today. A few of the many ways that organophosphates can affect the human body include interfering with the way testosterone communicates with cells, lowering testosterone, and altering thyroid hormone levels. Avoid it: Buy organic produce and use EWG’s Shopper’s Guide to Pesticides in Produce, which can help you find fruits and vegetables with the fewest pesticide residues (www.ewg.org/foodnews/).
- Glycol ethers: Shrunken testicles have developed in rats exposed to these chemicals which are common solvents in paints, cleaning products, brake fluid, and cosmetics. The European Union says that some of these chemicals “may damage fertility or the unborn child.” Studies of painters have linked exposure to certain glycol ethers with blood abnormalities and lower sperm counts. Children exposed to glycol ethers from paint in their bedrooms had substantially more asthma and allergies. Avoid it: Refer to EWG’s Guide to Healthy Cleaning (www.ewg.org/guides/cleaners/) and avoid products with ingredients such as 2-butoxyethanol (EGBE) and methoxydiglycol (DEGME).
References:
- “Dirty Dozen List of Endocrine Disruptors: 12 Hormone-Altering Chemicals and How to Avoid Them.” Environmental Working Group (EWG). 10/28/13.
- ATSDR (Agency for Toxic Substances and Disease Registry). 2004. Toxicological profile for polybrominated biphenyls and polybrominated diphenyl ethers. http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=529&tid=94
- ATSDR (Agency for Toxic Substances and Disease Registry). 2009. Public Health Statement for Perfluoroalkyls. Agency for Toxic Substances and Disease Registry, Division of Toxicology and Environmental Medicine. May 2009. http://www.atsdr.cdc.gov/toxprofiles/tp200-c1-b.pdf
- Blount BC, Pirkle JL, Oserloh JD, Valentin-Blasini L, Caldwell KL. 2006. Urinary perchlorate and thyroid hormone levels in adolescent and adult men and women living in the Unites States. Environmental Health Perspectives 114(12): 1865-71.
- Buck Louis GM, Sundaram R, Schisterman EF, Sweeney AM, Lynch CD, Gore-Langton RE et al. 2012. Heavy metals and couple fecundity, the life study. Chemisphere 87(11): 1201-7.
- Corpas I, Castillo M, Marquina D, Benito MJ. 2002. Lead intoxication in gestational and lactation periods alters the development of male reproductive organs. Ecotoxicology and Environmental Safety 53(2): 259-66.
- De Coster S, van Larebeke N. 2012. Endocrine-disrupting chemicals: associated disorders and mechanisms of action. Journal of Environmental and Public Health Article ID 713696.http://www.hindawi.com/journals/jeph/2012/713696/cta/
- Department of Health and Human Services, Public Health Service. September 2004.http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=529&tid=94
- Dearth RK, Hiney JK, Srivastava V, Burdick SB, Bratton GR, Dees WL. 2002. Effects of lead (Pb) exposure during gestation and lactation on female pubertal development in the rat. Reproductive Toxicology 16(4): 343-52.
- Du G, Hu J, Huang H, Qin Y, Han X, Wu D, et al. 2013. Perfluorooctane sulfonate (PFOS) affects hormone receptor activity, steroidogenesis, and expression of endocrine-related genes in vitro and in vivo. Environmental Toxicology and Chemistry 32(2): 353-60.
- EPA (U.S. Environmental Protection Agency). 2010. Consumer Factsheet on: Dioxin. U.S. Environmental Protection Agency. August 2010. http://cfpub.epa.gov/ncea/CFM/nceaQFind.cfm?keyword=Dioxin
- EPA (U.S. Environmental Protection Agency). 2012. Emerging Contaminants Fact Sheet – Perfluorooctane Sulfonate (PFOS) and Perfluorooctanoic Acid (PFOA). U.S. Environmental Protection Agency. May 2012.http://www.epa.gov/fedfac/pdf/emerging_contaminants_pfos_pfoa.pdf
- EPA (U.S. Environmental Protection Agency). 2013. Consumer Factsheet on: Atrazine. U.S. Environmental Protection Agency. January 2013. http://www.epa.gov/oppsrrd1/reregistration/atrazine/atrazine_update.htm
- EPA (U.S. Environmental Protection Agency). 2013. Consumer fact sheet on: GLYCOL ETHERS. U.S. Environmental Protection Agency. October 2013. http://www.epa.gov/ttnatw01/hlthef/glycolet.html
- EWG (Environmental Working Group). 2003. Suspect Salads. Toxic Rocket Fuel Fond in Samples of Winter Lettuce. http://www.ewg.org/research/suspect-salads
- EWG (Environmental Working Group). 2003. PFCs: Global Contaminants.
- http://www.ewg.org/research/pfcs-global-contaminants
- EWG (Environmental Working Group). 2004. Rocket Fuel Contamination in California Milk.http://www.ewg.org/research/rocket-fuel-cows-milk-perchlorate
- Fan W, Yanase T, Morinaga H, Gondo S, Okabe T, Nomura M, et al. 2007. Atrazine-induced aromatase expression is SF-1 dependent: implications for endocrine disruption in wildlife and reproductive cancers in humans. Environmental Health Perspectives 115(5): 720-727.
- FDA (Food and Drug Administration). 2013. Survey Data on Perchlorate in Food – 2005/2006 Total Diet Study Results.
- http://www.fda.gov/Food/FoodborneIllnessContaminants/ChemicalContaminant…
- Giammona CJ, Sawhney P, Chandrasekaran Y, Richburg JH. 2002. Death receptor response in rodent testis after mono-(2-ethylhexyl) phthalate exposure. Toxicology and Applied Pharmacology 185(2): 119-27.
- Gilbert ME, Rovet J, Chen Z, Koibuchi N. 2012. Developmental thyroid hormone disruption: prevalence, environmental contaminants and neurodevelopmental consequences. Neurotoxicology 33(4): 842-52.
- Hardin BD, Goad PT, Burg JR. 1986. Developmental toxicity of diethylene glycol monomethyl ether (diEGME). Fundamental and Applied Toxicology: Official Journal of the Society of Toxicology 6(3):430-9.
- Hayes TB, Stuart AA, Mendoza M, Collins A, Noriega N, Vonk A. 2006. Characterization of atrazine-induced gonadal malformations in african clawed frogs (Xenopus laevis) and comparisons with effects of an androgen antagonist (cyproterone acetate) and exogenous estrogen (17β estradiol): support for the demasculinization/feminization hypothesis. Environmental Health Perspectives 114(Suppl 1): 134-141.
- Hayes TB, Khoury V, Narayan A, Nazir M, Park A, Brown T, et al. 2010. Atrazine induces complete feminization and chemical castration in male African clawed frogs (Xenopus laevis). Proceedings of the National Academy of Sciences of the United States of America 107(10): 4612-4617.
- Iavicoli I, Fontana L, Bergamaschi A. 2009. The effects of metals as endocrine disruptors. Journal of Toxicology and Environmental Health Part B, Critical Reviews 12(3): 206-23.
- INSERM (Institut national de la santé et de la recherche médicale). 2006. Collective Expert Report: Glycol ethers: New toxicological data.
- Kato S, Fujii-Kuriyama Y, Ohtake F. 2007. A new signaling pathway of dioxin receptor ligands through targeted protein degradation. Alternatives to Animal Testing and Experimentation 14(special issue): 487-494.
- Kitamura S, Suzuki T, Ohta S, Fujimoto N. 2003. Antiandrogenic activity and metabolism of the organophosphorus pesticide fenthion and related compounds. Environmental Health Perspectives 111(4):503-8.
- Kitamura S, Sugihara K, Fujimoto N, Yamazaki, T. 2011. Organophosphates as Endocrine Disruptors. Anticholinesterase pesticides: metabolism, neurotoxicity, and epidemiology (eds T. Satoh and R. C. Gupta), John Wiley & Sons, Inc., Hoboken, NJ, USA.
- Lacasaña M, López-Flores I, Rodríguez-Barranco M, Aguilar-Garduño C, Blanco-Muñoz J, Pérez-Méndez O et al. 2010. Association between organophosphate pesticides exposure and thyroid hormones in floriculture workers. Toxicology and Applied Pharmacology 243(1):19-26.
- Laks DR. 2010. Luteinizing hormone provides a causal mechanism for mercury associated disease. Medical Hypotheses 74(4): 698-701.
- Liao C, Kannan K. 2011. Widespread occurrence of bisphenol A in paper and paper products: implications for human exposure. Environ Sci. Technol. 45(21): 9372-9.
- Lilienthal H, Hack A, Roth-Härer A, Grande SW, Talsness CE. 2006. Effects of developmental exposure to 2,2′,4,4′,5-pentabromodiphenyl ether (PBDE-99) on sex steroids, sexual development, and sexually dimorphic behavior in rats. Environmental Health Perspectives 114(2): 194-201.
- Main KM, Kiviranta H, Virtanen HE, Sundqvist E, Tuomisto JT, Tuomisto J, Vartiainen T, Skakkebaek NE, Toppari J. 2007. Flame retardants in placenta and breast milk and cryptorchidism in newborn boys. Environmental Health Perspectives 115(10): 1519-26.
- MDH (Minnesota Department of Health). 2006. Consumer Factsheet on: Dioxins. Minnesota Department of Health. October 2006. http://www.health.state.mn.us/divs/eh/risk/chemhazards/dioxins.html
- Meeker JD, Ferguson KK. 2011. Relationship between urinary phthalate and bisphenol A concentrations and serum thyroid measures in U.S. adults and adolescents from the National Health and Nutrition Examination Survey (NHANES) 2007-2008. Environmental Health Perspectives 119(10): 1396-402.
- Mocarelli P, Gerthoux PM, Needham LL, Patterson DG Jr, Limonta G, Falbo R, et al. 2011. Perinatal exposure to low doses of dioxin can permanently impair human semen quality. Environmental Health Perspectives 119(5): 713-718.
- Nagano K, Nakayama E, Oobayashi H, Nishizawa T, Okuda H, Yamazaki K. 1984. Experimental studies on toxicity of ethylene glycol alkyl ethers in Japan. Environmental Health Perspectives 57:75-84.
- Patisaul HB, Roberts SC, Mabrey N, McCaffrey KA, Gear RB, Braun J, Belcher SM, Stapleton HM. 2013. Accumulation and endocrine disrupting effects of the flame retardant mixture firemaster® 550 in rats: an exploratory assessment. Journal of Biochemical and Molecular Toxicology 27(2): 124-36.
- Post GB, Cohn PD, Cooper KR. 2012. Perfluorooctanoic acid (PFOA), an emerging drinking water contaminant: a critical review of recent literature. Environmental Research 116(24): 93-117..
- Rogers JA, Metz L, Yong VW. 2013. Review: endocrine disrupting chemicals and immune responses: a focus on bisphenol-A and its potential mechanisms. Molecular Immunology 53(4): 421-30.
- Rossi-George A, Virgolini MB, Weston D, Cory-Slechta DA. 2009. Alterations in glucocorticoid negative feedback following maternal Pb, prenatal stress and the combination: a potential biological unifying mechanism for their corresponding disease profiles. Toxicology and Applied Pharmacology 234(1): 117-27.
- Rubin BS. 2011. Bisphenol a: an endocrine disruptor with widespread exposure and multiple effects. The Journal of Steroid Biochemistry and Molecular Biology 127(1-2): 27-34.
- Soldin OP, Braverman LE, Lamm SH. 2001. Perchlorate clinical pharmacology and human health: a review. Therapeutic Drug Monitoring 23(4): 316-31. Review.
- Stanko JP, Enoch RR, Rayner JL, Davis CC, Wolf DC, Malarkey DE, Fenton SE. 2010. Effects of prenatal exposure to a low dose atrazine metabolite mixture on pubertal timing and prostate development of male Long-Evans rats. Reproductive Toxicology 30(4): 540-9.
- Tonacchera M, Pinchera A, Dimida A, Ferrarini E, Agretti P, Vitti P et al. 2004. Relative potencies and additivity of perchlorate, thiocyanate, nitrate, and iodide on the inhibition of radioactive iodide uptake by the human sodium iodide symporter. Thyroid: Official Journal of the American Thyroid Association 14(12): 1012-9.
- Walter H. Watson, James D. Yager. 2007. Arsenic: extension of its endocrine disruption potential to interference with estrogen receptor-mediated signaling. Toxicological Sciences 98(1): 1-4.
- Wolff J. 1998. Perchlorate and the thyroid gland. Pharmacology Review 50(1): 89-105.
- Wolstenholme JT, Rissman EF, Connelly JJ. 2011. The role of bisphenol A in shaping the brain, epigenome and behavior. Hormones and Behavior 59(3): 296-305.
- Ya Wen Chen, Ching Yao Yang, Chun Fa Huang, Dong Zong Hung, Yuk Man Leung, Shing Hwa Liu. 2009. Heavy metals, islet function and diabetes development. Islets 1(3): 169-176.
- Yamano T, Noda T, Shimizu M, Morita S, Nagahama M. 1993. Effects of diethylene glycol monomethyl ether on pregnancy and postnatal development in rats. Archives of Environmental Contamination and Toxicology 24(2): 228-35.
- Zhu X, Kusaka Y, Sato K, Zhang Q. 2000. The endocrine disruptive effects of mercury. Environmental Health and Preventative Medicine 4(4): 174-83
- Zota AR, Park JS, Wang Y, Petreas M, Zoeller RT, Woodruff TJ. 2011. Polybrominated diphenyl ethers, hydroxylated polybrominated diphenyl ethers, and measures of thyroid function in second trimester pregnant women in California. Environmental Science & Technology 45(18): 7896–7905.
{ Comments on this entry are closed }